Prevalence and Risk Factors for Skin Diseases Among Philippine National Police Personnels in Camp Crame, Quezon City, Philippines
Abigael T1* Villanueva, MD1,2, Gracia B. Teodosio MD, FPDS1, Ma.Teresita G. Gabriel, MD, FPDS1, Alexander R. Castillo, MD, FPDS1, Gisella U. Adasa, MD, FPDS1, Kristy Elleza R. Evangelista, MD1,Pauline Consuelo R. Velasco, MD1
1 Department of Dermatology, Research Institute for Tropical Medicine, Muntinlupa City, Philippines.
2 Philippine National Police, Health Service, Camp Crame, Quezon City, Philippines.
*Corresponding Author: Dr Abigael T Villanueva-Daniel, Department of Dermatology, Research Institute for Tropical Medicine, Muntinlupa City, Philippines, Tel: (02)8723-0401; Fax: (02)8723-0401; E-mail:iamabbey2000@yahoo.com
Citation: Abigael T. Villanueva, Gracia B. Teodosio, Ma Teresita, G. Gabriel, Alexander R Castillo, et al. (2023 Prevalence and Risk Factors for Skin Diseases Among Philippine National Police Personnels in Camp Crame, Quezon City, Philippines. J Dermatol & Ther 3: 118.
Received: April 11, 2023; Accepted: April 18, 2023; Published: April 22, 2023.
Copyright: © 2023 Abigael T Villanueva-Daniel, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Background
The Philippine government as stated in the 1987 Constitution has emphasized the need for national security and maintenance of peace and order in nation building. It fully recognizes that the lack of these may impact the economy and subsequently adversely affect the progress and development of the country. To ensure that this policy is enforced, the Philippine Constitution also states a provision for the establishment of a police force with the primary task of ensuring national security, the Philippine National Police (PNP). Philippine National Police (PNP), as the premier law enforcing agency is at the forefront in ensuring internal peace and order in the country. For the first time in the country, a baseline study on the prevalence and risk factors for common skin diseases among Philippine National Police personnel was conducted on the National Headquarters of the PNP from March 1 to August 31, 2016.

Significance of the Study
Given this tremendous responsibility of the police force, ensuring their optimum health should be a priority. Skin disease is an important health concern which is often overlooked but may impact work performance of the PNP and on a larger scale, affect national security. To date, no published study has been tracked to investigate skin diseases in the PNP. This research is the first step in addressing the common skin diseases among PNP. It aims to determine the prevalence and risk factors of common skin diseases among PNP officers. Better understanding of this is necessary to develop interventions for prevention and providing focused dermatologic health care services to the PNP.
Objectives of the Study
This pioneering study sought to determine the prevalence and specific types of skin diseases and their associated risk factors among police officers in Camp Crame, Quezon City, Philippines. To develop effective treatment plans and preventive measures for common skin diseases among PNP personnel. To have cost effective treatment for common skin diseases among PNP personnel.
Materials and Methods
Using a cross-sectional analytic study design, data were obtained from 384 randomly selected participants through self-administered questionnaires and skin examination performed by qualified dermatologists.
Results
Out of the 384 uniformed PNP personnel who participated in this study, 307 were found to have at least one skin disease thus resulting to skin disease prevalence of 80%. Among the general types of skin disease, dermatitis and eczemas ranked first with an estimated prevalence of 29.7% followed by pigmentary disorder (19.0%) and disorder of the skin appendage (17.2%). Among the specific types of skin disease, the most prevalent are melasma, acne and verruca plana (17.4%, 14.6% and 8.9%, respectively). Age, gender, position and years of service in the PNP, place of residence and work, and hygienic practices were found to be associated with various skin diseases. The prevalence of skin disease was found to increase significantly with the number of personal items shared with others. Lower composite hygiene score was associated with having at least one (non-communicable) skin disease.
Figure 1: Overall Prevalence of Skin Disease among PNP officers.
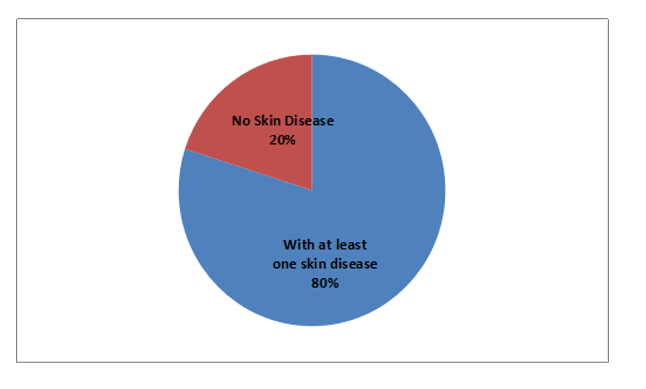
Out of the 384 police officers included in this study, 307 were found to have at least one skin disease resulting to an overall skin disease prevalence of 80%.
Figure 2: Prevalence of Communicable and Non-Communicable Skin Diseases.
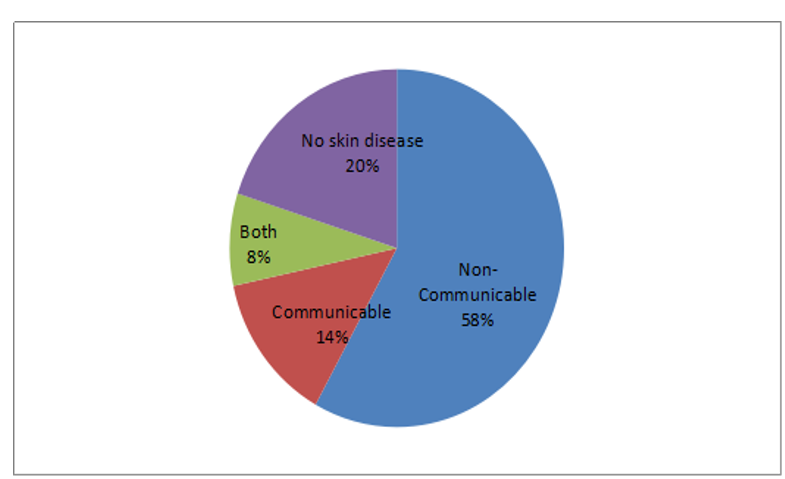
Among 307, 223 participants (58%) had only non-communicable skin disease findings, 52 participants (14%) had only communicable skin disease findings and 32 participants (10%) had both non-communicable and communicable skin disease findings.
Figure 3: Prevalence of Major Categories of Non-Communicable Skin Diseases.
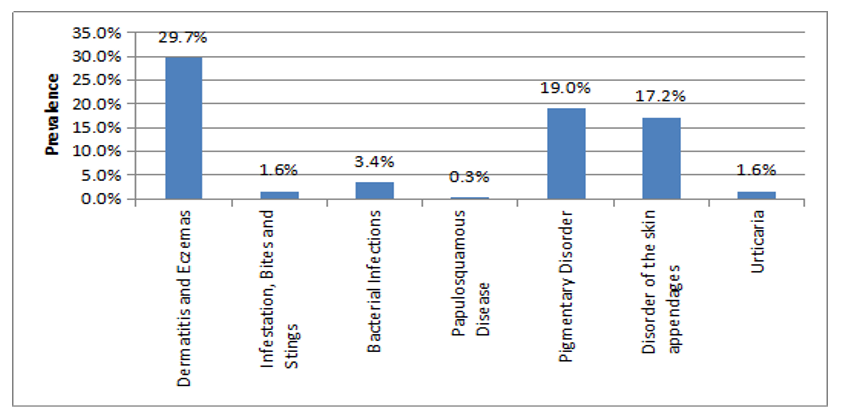
Dermatitis and eczemas ranked first which was present in 114 participants resulting in a prevalence of 29.7%. This was followed by pigmentary disorders having been found in 73 participants and a prevalence of 19.01%. Disorders of skin appendages were found in 66 participants and a prevalence of 17.2%.
Figure 4: Prevalence of Major Categories of Communicalble Skin Diseases.
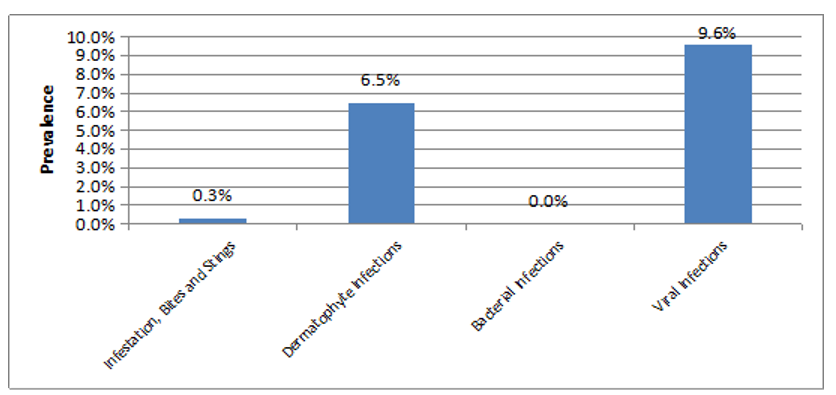
Viral infection was present in 37 participants resulting in a prevalence of 9.6%.
This was followed by dermatophyte infections having been present in 25 participants and a prevalence of 6.5%. Disorders of infestation, bites and stings were found in 1 participant and a prevalence of 0.3%. Communicable bacterial infections were not seen in any of the participants.
Discussion
Dermatologic diseases pose one of the most frequent health problems among police personnel. In our study, every 8 out of 10 police officers have at least one skin disease with an overall prevalence of 80%. Majority of those with skin findings had non-communicable type of skin disease with an average of 7 out of 8 police officers having this. Although they may cause few fatalities, this has a significant role in combative performance, troop morbidity and poor morale of the police personnel. Throughout history, skin diseases have produced significant morbidity during active police service. Among 384 patients included in the study, dermatitis and eczema accounted for the majority of skin referrals. Contributory factors were found to be the following: heat and humidity, occlusive effect of the military clothing protective gear, difficulty of maintaining personal hygiene, cramped living conditions and the stress of deployment. These risk factors were affirmed in our study correlating skin disease and personal hygiene, age, gender, years of service, place of residence and place of work (significance p<.05).
Among the dermatitis and eczemas, the most striking finding was the prevalence of seborrheic dermatitis which was 8.1%. This could be explained by the interaction of several factors such as immune dysfunction, emotional stress and host susceptibility. This was followed by atopic and dyshidrotic dermatitis as the most common skin disease in this category. These skin findings are known to be affected by factors of increase in age and physical factors such as variations in humidity and temperature. This was positively correlated in the study findings wherein skin diseases of eczema and dermatitis were significantly seen (significance p<.05) in the risk factors for increase in age, male gender and increase years of service. This has also been associated to place of residence of home and place of work as field which may be further explained by the variable environmental exposure to irritant and allergen, humidity and temperature present at home (as compared to barracks) as place of residence and field work (as compared to office work) as place of work.
Pigmentary disorders were the second most common non- communicable skin disease having been present in 19.01% of the participants. Under this category of skin disease, melasma was seen in the majority with a 17.4% prevalence. Female gender, genetic and hormonal influences in combination with sun exposure are key factors in the pathogenesis of melasma. This was positively correlated in our study wherein this was significantly seen (significance p<.05) in the risk factors of increase in age, female sex and increase of years in service as well as those with more frequent bathing practices and office work. The higher incidence in females may be attributed to hormonal influences such pregnancy, use of oral contraceptive pills and use of cosmetics. Hygiene practices of more frequent bathing and office work assignment may be explained by the habit of less frequent sunscreen application with no reapplication. At the background of this is the fact that lesser sun exposure is present with indoor work as opposed to field work. Disorder of the skin appendages was the third most common non-communicable skin disease in police officers with a prevalence of 17.2%. The current study showed acne to be a common skin problem in the police personnel with a prevalence of 14.6% and with a mean age of 34.5 years old. The presence of acne in the adult age may be due to the fact that they belong to a class society (police force), where stress can contribute to the aggravation of acne. This study showed that urticaria was seen in a small number of police officer with a prevalence of 1.3% and with a mean age of 35.2 years old. Other risk factors associated to this is the lower years of service. This may be explained by the aggravating factor of stress common in this age group. Surprisingly, a significant amount of police officers who had urticaria were found to have bed bugs in their sleeping area.
A smaller percentage of the police officers were seen with communicable skin diseases having an average of 3 out of 8 policemen having this. Majority of these have viral infections with a prevalence of 9.6% followed by dermatophyte infections with a prevalence of 6.5%. In general, communicable skin diseases are associated with factors of decrease immunity, poor hygiene and environmental exposure related to spread of disease. These risk factors were affirmed in our study correlating skin disease and rank, hygiene practices and place of residence (significance p<.05). Viral wart with a prevalence of 8.9% was the most common viral infection in the military force. Interestingly, the high prevalence was increased significantly with commissioned officers. This high prevalence might be due to sharing of personal items (significance p< 0.005%).
Fungal infection of the skin was the most common infectious diseases found in on both military and police troops in foreign studies. In these studies, tinea pedis was the most common fungal infection seen. In a cohort study done in Algeria and Israel, fungal infection was associated with the increase years of service and male gender, but no association was seen with hygiene practices. In our study, fungal infection with 9% prevalence was not related to smoking, age, gender and years of service. Aggravating factors that have caused the disease may be related to communal living, occlusive shoes, foot trauma and poor hygiene. This was shown in our study with a prevalence of dermatophyte infection which was 28.6% for those staying the in the communal residence (barracks).
Limitations
Due to the cross-sectional study design, this study cannot quantify the risk of developing skin disease in the study population. That would be possible only through a cohort study design, either retrospective or prospective, as long as there is baseline information on the status of the police officers in terms of the various skin diseases at the start of their PNP service.
Conclusion
Cutaneous diseases in police troops have been recognized as a significant cause of morbidity. In our study, eczemas, acne, fungal infection and verruca showed high prevalence in the police force. These diseases are not life threatening and incapacitating, however they may severely affect the daily activities and performance of the police troops. There were many other skin diseases detected during examination like urticaria and insect bite allergies which may be underestimated due to its transient appearance of symptoms. The knowledge of the spectrum of dermatologic diseases in police troops serves as an important planning guidance in the appropriate medical diagnosis management of skin diseases. Proper management of skin disease would therefore influence significantly the quality of the lives of the police troops in the combative environment and in the barracks. In addition, intensive information campaigns on its existence in the police troop, provision of protective garments, maintenance of cleanliness in the communal home and personal hygiene should be properly addressed.
References
1. The (1987) Constitution of the Republic of the Philippines, Article II, Section 5 Philippine National Police. [modified 2016 Aug 21; cited 2017 Sept 10].
2. Philippine Statistics Authority (2016) [modified 2016 Sept 19; cited 2017 Sept 10].
3. Philippine Statistics Authority. [modified 2016 May 19; cited 2017 Sept 10]. Highlights of the Philippine Population 2015 Census of Population. Available from: https://www.psa.gov.ph/content/highlights- philippine-population-2015-census-population
4. McGraw, T A, & Norton, S A (2009) Military aeromedical evacuations from central and southwest Asia for ill- defined dermatologic diseases. Archives of dermatology 145: 165-170.
5. Gelman, A, Norton, S A, Valdes-Rodriguez, R, Yosipovitch, G et al. (2015) A Review of Skin Conditions in Modern Warfare and Peacekeeping Operations. Military medicine 180: 32-37.
6. Henning, J S, Firoz, B F (2010) Combat dermatology: the prevalence of skin disease in a deployed dermatology clinic in Iraq. Journal of drugs in dermatology: JDD 9: 210-214.
7. Raza, N, Agha, H, Suhail, M (2014) Frequency and Pattern of Skin Diseases among Uniformed Personnel at United Nations Level III Hospital-Darfur, Sudan. Pakistan Armed Forces Medical Journal, 64: 84-87.
8. Suresh, K P, Chandrashekara, S (2012) Sample size estimation and power analysis for clinical research studies. Journal of human reproductive sciences 5: 7.
9. Turabelidze G, Lin M, Wolkoff B, Dodson D, Gladbach S, et al. (2006) Personal hygiene and methicillin-resistant Staphylococcus aureus infection. Emerg Infect Dis 12: 422-7.
10. Whiteman DC, Stickley M, Watt P, Hughes MC, Davis, et al. (2006) Anatomic site, sun exposure, and risk of cutaneous melanoma. Journal of Clinical Oncology 24: 3172-3177.
11. Goldsmith L, Katz S, Gilchrest B, Paller AS, Leffell D, et al. (2012) Fitzpatrick's Dermatology in General Medicine, 8th Edition. New York: McGraw-Hill.
12. Naldi L (2010) Seborrhoeic dermatitis. BMJ Clin Evidii 1713.
13. Selvaag E (2000) Skin disease in military personnel. Military medicine 165: 193-194.
14. Lagda LE, Visitacion LR (2002) The prevalence of tinea pedis and an evaluation of some factors related to its development among uniformed PNP personnel at Camp Catitipan, Davao City. J Phil Soc Cutaneous Med 2: 37-43.
15. Collier CN, Harper JC, Cantrell WC, Wenquan W, Foster KW, et al. (2008) The prevalence of acne in adults 20 years and older. Journal of the American Academy of Dermatology 58: 56–59.
