Prevalence of Metabolic Syndrome and Associated Factors in a Peri-urban Population in Uganda. The MEPI CVD survey.
Nabunnya Yvonne Brenda1*, Ssinabulya Isaac1, Dr. Joanita Nankabirwa1, Kayima James1
1 Makerere University college of health sciences, Uganda.
*Corresponding Author: Nabunn ya Yvonne Brenda, Makerere University college of health sciences, Uganda, Tel: (+256) 41 4530 020; Fax: +256) 41 4530 020; E-mail: yvonne.nabunnya@gmail.com
Citation: Nabunnya Yvonne Brenda, Ssinabulya Isaac, Dr. Joanita Nankabirwa, Kayima James (2023) Prevalence of Metabolic Syndrome and Associated Factors in a Peri-urban Population in Uganda. The MEPI CVD survey. Arch Mol Med & Gen 3: 119.
Received: March 29, 2023; Accepted: April 08, 2023; Published: April 17, 2023.
Copyright: © 2023 Nabunnya Yvonne Brenda, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Background: Metabolic syndrome (MetS) is an key contributor to cardiovascular disease and is defined by the presence of any 3 or more of the following features (central obesity, raised triglycerides, reduced high density lipoprotein cholesterol (HDL-c), raised low density lipoprotein (LDL-c), raised blood pressure, raised fasting blood glucose) as mentioned by the international diabetic federation (IDF)(1) or National Cholesterol Educational Program (NCEP- ATP III)(2). A person with MetS is twice as likely to develop cardiovascular disease and five times as likely to develop diabetes mellitus. The increasing prevalence of cardiovascular disease worldwide requires urgent detection of this risk factor whose prevalence ranges between17% and 50% in some African countries. In Uganda, the prevalence of MetS has not been documented (4) although the prevalence of its components has been published. For example, the prevalence of hypertension ranges from 24-27% (4, 5, 6), while dyslipidaemias have been found to be 6.7% by the national non communicable diseases survey (7, 8). Interestingly 76% of those with hypertension and 89%of those with diabetes were not on any treatment.
Objective: To determine the prevalence and associated factors of MetS in a peri-urban Ugandan population.
Methods: This was part of the MEPI survey. A cross sectional study carried out in Wakiso district and participants were recruited from two sub counties Nansana and Busukuma of urban and rural status, in peri urban Uganda. 4902 participants were recruited using the WHO STEP-Wise approach to non-communicable disease surveillance. Metabolic syndrome was defined by using NCEP-ATPIII and IDF-2006. Adults 18 years and above who consented to participate in the study were recruited. Demographic and clinical data was collected using a questionnaire. Biophysical measurements and blood chemistries were measured. This data was analyzed using stata version11.
Results: The prevalence of MetS was found to be 8.4% in males and 15.3% in females using the NCEP-ATPIII definition, while it was found to be 13.8% in males and 26.4% in females using the IDF definition. Risk factors include older age, female sex, and having a family history of high blood pressure. Low HDL-c and high blood pressure are the commonest components of metabolic syndrome found in this survey.
Conclusion and Recommendation: The prevalence of MetS is high and is associated with increasing age, female gender, and being a rural dweller. Early screening of risk factors to curtail cardiovascular risk, implementation of both pharmacological and non-pharmacological controls will significantly reduce their risk to cardiovascular disease.
Key words
Metabolic Syndrome, Peri-Urban Population, Uganda.
Background
The prevalence of non-communicable diseases (NCD) is on the increase worldwide . According to the world health report 2003 cardiovascular disease (CVD) accounts for 17 million deaths worldwide (). The risk factors to CVDs are individually also on the increase. The prevalence of metabolic syndrome has been reported to be 8% in India, 24% in USA. In Africa a few studies have reported prevalence of 17% and 25% in Nigeria (ref). In Uganda the National non communicable disease risk survey found high prevalence of components of metabolic syndrome for example 1 in 4 adults were found to suffer from hypertension, 3.3% found with diabetes, 6.7% found with high total cholesterol and 4.6% obese. The prevalence of MetS increases to as high as 50% in those with impaired glucose tolerance and it’s even higher in those with diabetes mellitus (Ref). This trend has been attributed to decreased physical activity, substitution of traditional African diet for western diet. This high prevalence of CVD risk factors means that a considerable proportion of the population needs to be identified and connected to long term care. The prevalence of metabolic syndrome has been found more in females; it increases with age, and predominantly in urban dwellers. Metabolic syndrome increases cardiovascular risk particularly for coronary heart disease and stroke. Early identification and linking to care may delay or completely prevent progression to coronary heart disease or stroke. The aim of this study is to determine the prevalence and associated factors of metabolic syndrome in a peri urban population in Uganda. The aim of the study was to determine the prevalence of cardiovascular disease (CVD), to establish the prevalence of major CVD risk factors in the study population stated as smoking, alcohol consumption, physical inactivity, diets high in fats and less in fruits and vegetables, obesity, and dyslipidaemias and to assess the knowledge and perceptions of CVD and CVD major risk factors in the study population.
Methods
This was a cross-sectional community-based survey in two sub counties of Nansana and Busukuma in Wakiso district which are classified as urban and rural respectively. The households included were randomly generated from a census database at each site. The WHO recommended STEP-wise approach was followed as follows. 1. administration of the questionnaire 2. measurement of physical parameters such as weight, height, waist hip ratio, blood pressure and heart rate.3. Laboratory measurements including fasting blood glucose, Hb A1c , lipid parameters. Samples were stored for further studies. The target population was the combined population of Nansana and Busukuma sub counties of 134,800. Using multistage sampling at the Sub County, parish, and village level a sample size of 7000 study participants were to be recruited 5000 adults were interviewed. At the household level, one member per household aged 18 years or older who agreed to provide informed consent, was recruited, the questionnaire administered to them, physical anthropometric measurements such as weight, height, waist circumference, hip circumference and blood pressure were measured using a seca 762 weighing scale, a seca 214 portable stadiometer, a measuring tape and an omron automated sphygmomanometer model HEM-907, respectively. Blood samples were drawn for laboratory tests performed at MBN laboratory. Tests performed included, fasting blood sugar, total cholesterol total cholesterol, LDL cholesterol, HDL cholesterol, Data was collected using both paper questionnaire and electronic personal digital assistants by trained research assistants. This data was then downloaded to a Microsoft access database. Data was analyzed using stata version 11 for this study and the international diabetes Federation (IDF) and National cholesterol education program (NCEP-ATP111) definitions of metabolic syndrome were utilized. This study received approval from the school of medicine research and ethics committee of the college of health sciences Makerere University and from the National council for science and technology. From August 2012 to May 2013, eligible participants who consented to participate in the mepi cvd survey were recruited. Using the WHO step wise approach biophysical and chemistry information was collected.
Results
Results of 4902 participants are presented here. The mean age of participants in this study is 32 (SD) years in the urban population while it is 39 (SD) years in the rural population. Females represent 72 % of the participants from the urban population and 59% of those from the rural population. Of the participants from the urban population 27% are male and of those from the rural populations 40% are male. 62% of the participants from the urban setting were categorized as poor in terms of social economic status. 7% of participants from the rural setting were characterized as poor. 8% of participants from the urban population and 10% of participants from the rural population have a history of smoking, 9% of participants from the rural population and 16% of the urban participants have a history of consuming alcohol. 29% of participants have a family history of high blood pressure. (Table1).
Table 1: Participants socialand demographic characteristics.
|
|
Urban N=3,564 |
Rural N=1,338 |
Total |
|
Age-group(years) |
|
|
|
|
18-24 |
1,011 (28.4) |
237 (17.7) |
|
|
25-34 |
1,333 (37.4) |
340 (25.4) |
|
|
35-44 |
630 (17.7) |
305 (22.8) |
<0.0001 |
|
45-54 |
348 (9.8) |
219 (16.4) |
<0.0001 |
|
55-64 |
136 (3.8) |
99 (7.4) |
<0.0001 |
|
>65 |
106 (2.9) |
138 (10.3) |
<0.0001 |
|
Mean age |
<0.0001 |
||
|
Sex |
|
|
|
|
Male |
987 (27.7) |
540 (40.4) |
|
|
Female |
2,577 (72.3) |
798 (59.6) |
<0.0001 |
|
Social economic status |
|
|
|
|
Most Poor |
1,143 (32.1) |
105 (7.9) |
|
|
Poor |
1,011 (28.4) |
190 (14.2) |
<0.0001 |
|
Less poor |
623 (17.5) |
657 (49.1) |
<0.0001 |
|
Least poor |
787 (22.1) |
386 (28.9) |
<0.0001 |
|
Smoking |
|
|
|
|
Never smoked |
3,258 (91.4) |
1,193 (89.2) |
|
|
Previously smoked |
145 (4.1) |
46 (3.4) |
|
|
Currently smoking |
161 (4.5) |
99 (7.4) |
<0.0001 |
|
Alcohol |
|
|
|
|
No intake |
3,213 (90.2) |
1,117 (83.5) |
|
|
Mild intake |
94 (2.6) |
57 (4.3) |
|
|
Moderate intake |
172 (4.8) |
110 (8.2) |
<0.0001 |
|
Heavy intake |
85 (2.4) |
54 (4.0) |
|
|
Family history of high blood pressure |
|
|
|
|
No |
2,527 (70.9) |
1,052 (78.6) |
|
|
Yes |
1,037 (29.1) |
286 (21.4) |
<0.0001 |
The contributions of the different components of metabolic syndrome are as follows. Obesity was present in 5% females and 51% male according to the IDF definition as compared to 1% in males and 29% in females. Abnormal triglycerides were found in 21% in males and 19% in females, 55% males presented abnormal HDL cholesterol as compared to 46.7% females.43%males and 36% females presented with abnormal blood pressure measures. 18% males and 26% females were found with abnormal fasting blood sugar using the IDF definition while 7% males and 11% females were found with abnormal fasting blood sugar using the NCEP ATP111 ATPIII definition. The overall prevalence of metabolic syndrome is 13% using NCEP-ATPIII and 22% using the IDF definition. (Table 2).
Table 2: Prevalence of metabolic syndrome and its components by sex among study participants.
|
Variable |
Men(N=1,527) |
Women(N=3,375) |
P-value |
|
Waist circumference ≥94 cm for men or ≥80 cm for women (IDF) |
|||
|
Normal |
1,438 (94.2) |
1,649 (48.9) |
|
|
Obese |
89 (5.8) |
1,726 (51.1) |
<0.0001 |
|
Waist circumference ≥102 cm in men or ≥88 cm in women;(ATP 111) |
|||
|
Normal |
1,510 (98.9) |
2,396 (70.9) |
|
|
Obese |
17 (1.1) |
979 (29.1) |
<0.0001 |
|
Triglycerides ≥1.7 mmol/l [≥150mg/dl]; |
|||
|
Normal |
1,197 (78.4) |
2,712 (80.4) |
|
|
Abnormal |
330 (21.6) |
663 (19.6) |
|
|
(iii) HDL cholesterol (HDL-C), |
|||
|
Normal |
678 (44.4) |
1,798 (53.3) |
|
|
Abnormal |
849 (55.6) |
1,577 (46.7) |
<0.0001 |
|
Systolic BP ≥130mmHg and/or Diastolic BP ≥85 mmHg |
|||
|
Normal |
862 (56.5) |
2,146 (63.6) |
|
|
Abnormal |
665 (43.6) |
1,229 (36.4) |
<0.0001 |
|
FBG ≥6.1 mmol/l (ATP 111) |
|
|
|
|
<6.1 |
1,407 (92.1) |
2,996 (88.8) |
|
|
>6.1 |
120 (7.9) |
379 (11.2) |
<0.0001 |
|
Elevated fasting glucose ≥5.6 mmol/L or treatment of previously diagnosed diabetes (IDF) |
|||
|
Normal |
1,240 (81.2) |
2,498 (74.0) |
|
|
Abnormal |
287 (18.8) |
877 (26.0) |
<0.0001 |
|
MetS (NCEP-ATPIII definition) |
|||
|
None |
1,398 (91.6) |
2,860 (84.7) |
|
|
Present |
129 (8.4) |
515 (15.3) |
<0.0001 |
|
MetS (IDF definition) |
|
|
|
|
None |
1,316 (86.2) |
2,483 (73.6) |
|
|
Present |
211 (13.8) |
892 (26.4) |
<0.0001 |
Gender specific prevalence is 8% males and 15% females using the NCEP-ATPIII definition while it is 13% males and 26% females using the IDF definition. (Figure1)
Figure 1: Prevalence of metabolic syndrome (IDF)by sex.

Figure legend. Histogram showing metabolic syndrome predominantly more in females than males.
Associated risk factors include increasing age, female sex, low social economic status, alcohol consumption and family history of hypertension in order of importance. (Figure2).
Figure 2: Prevalence of metabolic syndrome (IDF) by age-group.
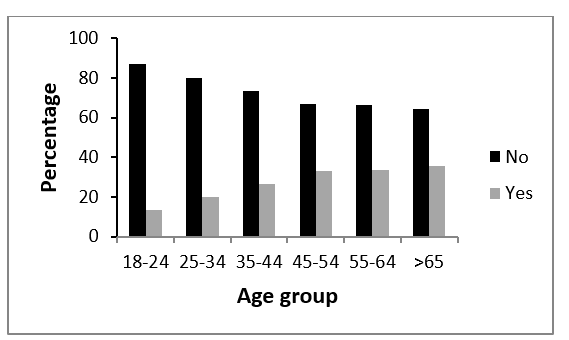
Figure legend. Prevalence of metabolic syndrome by age group showing increasing prevalence with increasing age.Of note was that 51% of females (IDF) as compared to 29% (ATP III), abnormal HDL is 55% in men and 46% in women, abnormal triglycerides 21% in females and 19% in males, fasting blood sugar more than 6.1(ATP III) is 7% in males and 11% in females while it is 18% in males and 26%in female (IDF).
Table 3: Association of selected risk factors with metabolic syndrome (IDF) among a peri urban population in Uganda.
|
Variable |
|
Un adjusted |
|
Adjusted |
|
|
|
Metabolic syndrome n, (%) |
OR |
p-value |
OR |
95% CI |
|
Age-group(years) |
|
|
|
|
|
|
18-24 |
165 (13.2) |
|
|
|
|
|
25-34 |
335 (20.1) |
1.6 (1.3 -1.9) |
<0.0001 |
1.6 (1.3 -1.9) |
<0.0001 |
|
35-44 |
250 (26.7) |
2.5 (2.0 – 3.2) |
<0.0001 |
2.5 (2.0 – 3.2) |
<0.0001 |
|
45-54 |
187 (33.0) |
3.4 (2.7 – 4.4) |
<0.0001 |
3.4 (2.7 – 4.4) |
<0.0001 |
|
55-64 |
79 (33.6) |
3.6 (2.6 – 5.1) |
<0.0001 |
3.6 (2.6 – 5.1) |
<0.0001 |
|
>65 |
87 (35.7) |
3.6 (2.6 – 5.1) |
<0.0001 |
3.6 (2.6 – 5.1) |
<0.0001 |
|
Sex |
|
|
|
|
|
|
Male |
211 (13.8) |
|
|
|
|
|
Female |
892 (26.4) |
2.0 (1.7 – 2.4) |
<0.0001 |
2.0 (1.7 – 2.4) |
<0.0001 |
|
Sub-county |
|
|
|
|
|
|
Nansana Town Council (urban) |
903 (25.3) |
|
|
|
|
|
Busukuma (rural) |
200 (14.9) |
0.4 (0.3 -0.5) |
<0.0001 |
0.4 (0.3 -0.5) |
<0.0001 |
|
Social economic status |
|
|
|
|
|
|
Poorest |
245 (19.6) |
|
|
|
|
|
Poor |
248 (20.7) |
1.1 (0.9 – 1.3) | 1.1 (0.9 – 1.3) | ||
|
Less poor |
287 (22.4) |
1.2 (1.0 – 1.5) | 1.2 (1.0 – 1.5) | ||
|
Least poor |
323 (27.5) |
1.2 (1.02 – 1.5) |
<0.0001 |
1.2 (1.0 – 1.5) | |
|
Smoking |
|
|
|
|
|
|
Never smoked |
1,012 (22.7) |
|
|
|
|
|
Previously smoked |
44 (23.0) |
|
|
||
|
Currently smoking |
47 (18.1) |
|
|
||
|
Alcohol |
|
|
|
|
|
|
No intake |
1,008 (23.3) |
|
|
|
|
|
Mild intake |
18 (11.9) |
0.5 (0.3 -0.8) | 0.5 (0.3 -0.8) | ||
|
Moderate intake |
46 (16.3) |
0.8 (0.5 -1 .1) | 0.8 (0.5 -1 .1) | ||
|
Heavy intake |
31 (22.3) |
1.2 (0.8 -1.9) | 1.2 (0.8 -1.9) | ||
|
Family history of high blood pressure |
|
|
|
|
|
|
No |
727 (20.3) |
|
|
|
|
|
Yes |
376 (28.4) |
1.3 (1.1 – 1.5) |
<0.0001 |
1.3 (1.1 – 1.5) |
Discussion
The prevalence of metabolic syndrome ranges between13% to 22% (NCEP-ATPIII and IDF respectively) the main risk factors are abnormal HDL-C, triglycerides, blood pressure, age, female gender, smoking, alcohol consumption, history of hypertension. The prevalence of metabolic syndrome predicted 25% of all new onset cardiovascular disease (CVD) and 10% to 20% of metabolic syndrome predicts diabetes (DM) framingham prediction for coronary heart disease in 10years. These methods provide practical tools to identify those at increased risk and controls put in place. It is noted that abnormal HDL-C and systolic blood pressure are prevalent in males while elevated waist circumference and Fasting blood glucose are prevalent in females.
Compared head-to-head the sensitivity and specificity of NCEP ATP 111 and IDF is.
Recommendations
The high prevalence of metabolic syndrome means that targeted risk control is necessary. The areas of intervention are both non-pharmacological and pharmacological. As observed above, targeted weight control through physical exercise has benefits of lower serum cholesterol, triglycerides, C- reactive protein and PAI-1 raises HDL-C, lowers blood pressure, blood glucose, and prevents insulin resistance. Thus, reduced morbidity and mortality from cardiovascular disease decreases the disease burden on the health care system. The approaches to prevention of obesity and metabolic syndrome through the promotion of healthy lifestyles glucose and saturated fats regulation can be widely implemented. Makerere University College of health sciences in collaboration with Mbarara University of science and technology, Uganda heart institute and case western reserve university have a specifically directed training program emphasizing CVD identification, control and management during training has been done.
Acknowledgement
Funding: Research reported in this publication was supported by the Fogarty International Center, the National Heart Lung and Blood Institute, and the Common Fund of the National Institutes of Health under Award Number R24 TW008861. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Author contribution: ………………………………………………….
