Role of Kamdudha Rasa and Drakshasava in Amalpitta W.S.R Gastritis
Nishu Raina1*
1 Dac, Guru Ravidas Ayurved University, VPO.Kharkan, Una Rd, Hoshiarpur, Punjab, India.
*Corresponding Author: Nishu Raina, Dac, Guru Ravidas Ayurved University, VPO.Kharkan, Una Rd, Hoshiarpur, Punjab, India., TEL: 8360083394/9419132548; FAX: ; E-mail:nishu.raina2010@gmail.com
Citation: Nishu Raina (2019) Role of Kamdudha Rasa and Drakshasava in Amalpitta W.S.R Gastritis. Medcina Intern 2019 3: 139
Copyright: :© 2019 Nishu Raina, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited
Received date: December 12, 2019; Accepted date: December 22, 2019; Published date: December 25, 2019.
Abstract
Globally For a long time, communicable diseases were the biggest killer diseases. But now, the trend is changing towards increased prevalence of chronic diseases with causative factors mostly related to diet and lifestyle. Among them, the nidana (causative factors) of Amlapitta, a gastrointestinal tract (GIT) disorder, has acquired majority of the share with causative factors like improper diet and habits, stress, spicy irritant food, oily foods, bakery products, etc. The World Health Organization - WHO has estimated that major percentage of the population in developing countries depends primarily upon herbal medicine for basic health care. In this rapidly growing civilisation and multi media technology, life becomes full of stress having more speed and accuracy is prime demands. So people neglect healthy food and are attracted towards the junk food. They are changing their diet pattern, life style and behavioural pattern. People are becoming more stressful with worry, tension and anxiety causing so many physchological disorders which hampers the digestion and is causing hyperacidity, gastritis, dyspepsia, peptic ulcer disorder and anorexia. All these pathological disorders covered under the broad umbrella of Amlapitta in Ayurveda. It is that disease which bears the direct impact of the dietic errors that a person indulges 80% of the top 10 life threatening disease of the world that are due to faults in dietary habits. In ayurveda Amlapitta cannot be correlated with one particular disease more precisely but it can be correlated with acid reflex syndrome which comprises of GERD, Gastritis, Acid Peptic disorder, hyper acidity etc. In ayurveda sign and symptoms of amalpitta mentioned by ayurveda stalwarts looks very similar to GERD and gastritis. In ayurvedic terminology, Agni (digestive fire) is considered as the protector of the human body while Ama (toxic) is the cause of disease. The main cause is the indiscretion in taking food which leads to three types of doshic (physical energies imbalance Vata Pitta Kapha) and these doshas are found in the grahini (duodenum) which is considered as the seat of the digestive fire or agni. It is also said that eating and fasting during indigestion leads to problems like acidity, heartburn, gastritis which is refered as amalpitta. Ayurveda follows its own unique philosophy and methodologies to address issues of health care and prescribes variety of simple therapies as also certain complex treatments that could comprise of single ingredients, poly-ingredient formulations and combination of drugs, diet, lifestyle changes and therapies like massages, fomentation therapies, enemas and several other cleansing procedures as well. In this research we will find the role of kamdudha rasa and drakshasava in the management of amalpitta and their probable mode of action and are ideally meant to be administered only after proper understanding of the ailment as per Ayurvedic diagnostics or nidan.
Keywords:
amalpitta,agni, dosha,gastritis, GERD
Introduction
For a long time, infectious diseases were the biggest killer diseases globally, but now the trend is changing toward increased prevelance of lifestyle disorders. The annavaha srotas that is the one that bears a direct impact of all the dietetic errors that a person indulges. Besides this, Improper if we are in hurry and we donot chew the food properly or hurriedly gulped rough and hard portions of food, they are not going to get digest properly. Many a times the simple agnimandya (decreased digestive fire), leads to vidagdhajirna (dyspepsia) in the initial stages and if it is neglected it can further lead to amalpitta (gastritis). Hence we can say that it is the disease which bears the direct impact of the dietic errors that a person indulges 80% of the top 10 life threatening disease of the world that are due to faults in dietary habits. Prevalence range of gastritis is of about 11 to 38.8% of world population. Malaysia, mexico, spain and yemen reported figures on the top quartile prevelance, whereas asain countries reported prevelance rate are in the lowest quartile. It is reported that out of total population of 7.6% of Indian subjects have significant GERD symptoms. Rapid socioeconomic development and westernization of asian life styles including diet change and increase in average BMI, are likely to be the key factors in charge in epidemiology. In ayurvedic terminology, in case of amalpitta, vitiation of pitta dosha occurs along with kapha dossa. Although amalpitta is an established entity from the time of “madhav nidan” and Although this disease as such is not described in any text of the brihitya, but a condition named as “vidagdha jeerna” can be compared with amalpitta to some extent.
Disease review
Synonyms: Pramilaka, Pitta visuchika- as.sa.su.5/27 indu. Commentary, and Amlika- su.su.42/9
Amalpitta is basically composed of two words Amla and pitta .When we talk about the term “amla” , then it refers to a particular type of taste equated with sour taste which causes excessive salivary secretion, while on the other hand, Pitta is a bodily chemical substance which is mainly responsible for the maintainence of the process of digestion, transformation and transmutation. On combining both these words, the term amalpitta implies to a disease or condition in which sourness of pitta gets increased. So in short we can say amalpitta is a disease caused due to vitiation of certain attributes of
1. Pitta like the Drava guna (fluidity) and Amla guna (sourness) causing vidagdhajirna at the initial stages and
2. Later causes inflammation and corrosion of the sleshmadhara kala of the amashaya that is corrosion of the sleshmadhara kala of the amashya that is mucous membrane of the stomach and duodenum.
Nidana: After careful screening and analysis of the etiological factors of Amlapitta , they may be discussed under four groups
1. The Aharaja Hetu (dietary factors): abhisyandi (heavy diet), atisingdha (unctuous), atiruksha (very coarse), apakwanna sevana (uncooked food), bhristadhanya sevana (fried paddy), iksuvikara sevana (sugar cane products), atiusna (very hot), atiamla (intake of excessive acidic diet), atitikshna (sharp substance intake),, atipanam (over drinking), katuanna pana (pungent diet and drinks), viruddhasana (incompatibile diet) etc are some of the faulty dietary factors that can result in amalpitta.
2. Viharaja Hetu (Habit factors): Atisnat (Taking excessive bath), Ati Avagahanat (Excessive swimming) , Bhuktwa Diwasvapnat (Sleeping in day time after meals) ,Vega Dhararam (Suppression of natural urges) and Shayya Prajagarae (Improper sleeping schedule) are some of the habits which results in the disturbance of the whole functioning of the body and in the long run, they will cause the disturbance of the equilibrium of Pitta and digestion which ultimately will lead to Amlapitta .
3. Manasika Hetu (Psychogenic factor): an abnormal psychology (in terms of anger, anxiety, greed etc) affects the physiology of digestion, resulting in
i. lesser secretion of the digestive juice
ii. digestive juices secreted at improper times or in excessive quantity.
All these factors, aggravates Pitta and gives rise to Amlapitta.
4. Agantuka Hetu (miscellaneous factors): Various types of incompatible substances, excess of Pitta aggravating factors like Katu, Amla, Vidahi etc and untimely consumption of food are the factors against the dietetic code which are directly responsible for the disturbances of Pitta.
Acid gastritis is nothing else but is the syndrome resulting from stress and strain which shows the important role being played by psychogenic factors in the production of Amlapitta.
Samprapti of amalpitta: Kashyapa, Madhava and Gananatha Sen have mentioned specific Samprapti of Amlapitta as follows. Over indulgence in above mentioned aetiological factors resulted in vitiation of Vata and Pitta Dosha resulting in Jatharagnimandya. Hence whatsoever food consumed, becomes Vidagdha cum Sukta and lies in the stomach stagnant .At this stage Vidagdhajirna manifests which is the Purvarupa of the disease. And the vitiation of Pitta and Sukta, which forms Pitta Amavisa Sammurchhana starts occurring. And in this way Amlapitta with its cardinal symptoms is then born and If not treated properly in this stage, the disease leads to Bhedavasta where the typical characteristic types like Urdhwaga, Adhoga etc. are differentiated. Although no specific Purvarupas of Amlapitta are mentioned, still Agnimandya and Ajirna are the successive stages towards the manifestation of Amlapitta and are practically observed in all the patients. Annavaha and Purishavaha Srotodusti symptoms can also be considered as Purvarupa of Amlapitta. Symptoms of Amlapitta have been described by Kashyapa, Madhava Kara & Harita. Later workers of Sangrahakala like Bhavamishra,Vangasen and Yogaratnakara have followed Madhavkar. The symptoms of Amlapitta as per Madhava are as Avipaka (indigestion), Kanthadaha (burning sensation), Klama (being tired), Tikta Amla Udgara (bitter & soul belching), Gaurava (laziness), Utklesha (nausea) and Hritdaha (burning sensation). While on the other hand Antrakujana, Vidbheda, Udara Admana, Hritshula etc are being added by kashyapa acharya.
Types of Amlapitta
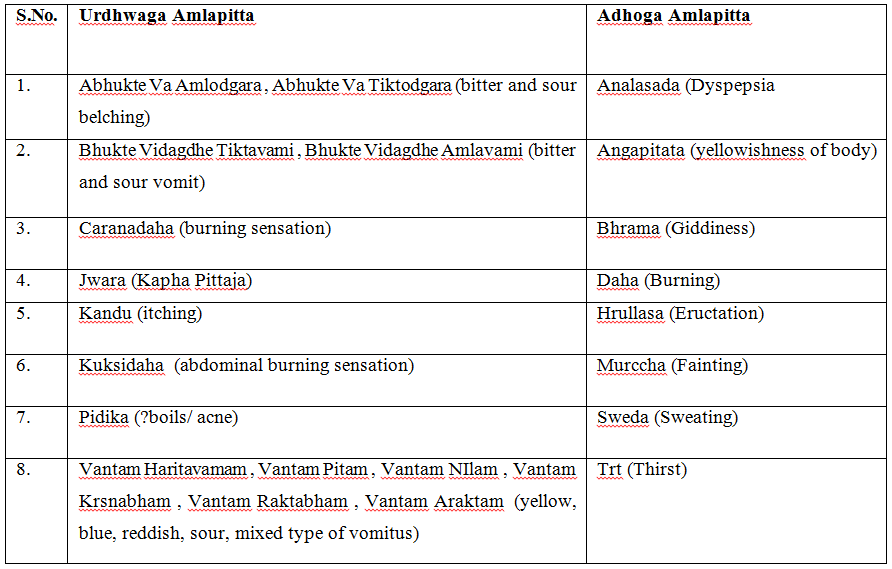
According to the Gati of Pitta, Madhava has described 2 types of Amlapitta Urdhvaga Amlapitta (NUD) and Adhoga Amlapitta
As per dosha involement: Table 1.
Table 1:
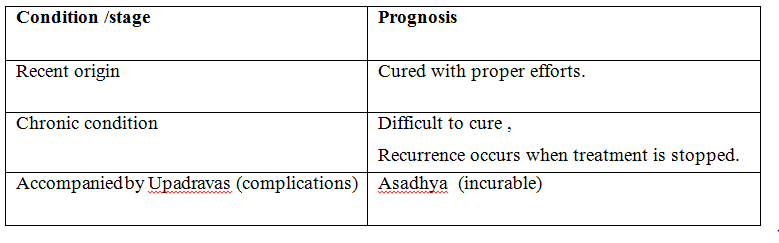
Sadhyasadhyata (Madhava): Table 2.
Table 2:
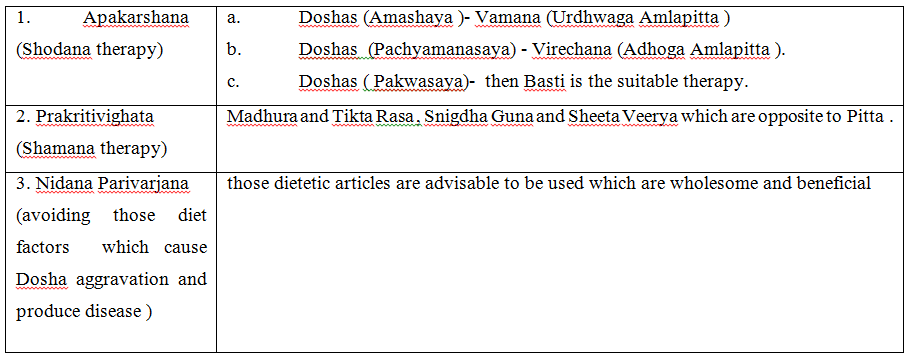
Chikitsa of Amlapitta (Charaka): Table 3.
Table 3:
Modern view
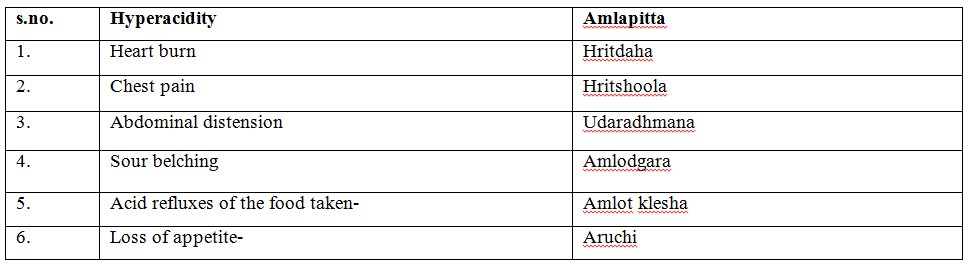
Some technical terms have been used to indicate an abnormal condition resembling to Amlapitta. These terms either explain the pathological condition of the disease or explain the characteristics of the disease. Table 4.
Table 4:
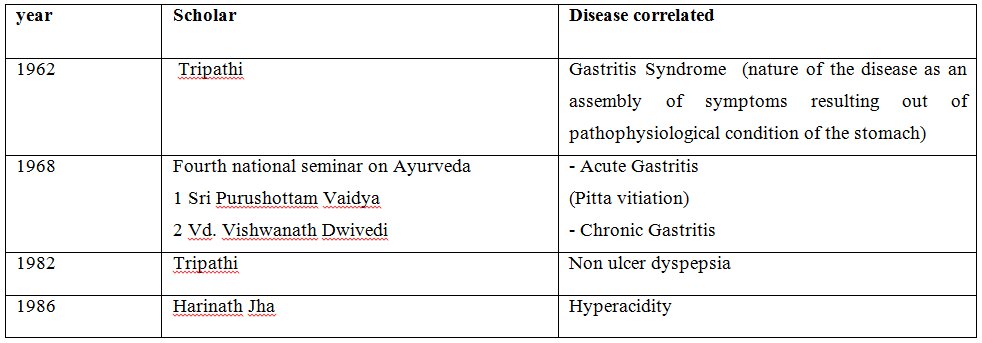
Showing correlation between Hyperacidity and Amlapitta. Table 5.
Table 5:
As explained earlier, any disease does not perfectly correlate with the aetiology, signs and symptomatology of Amlapitta. Some diseases show similarity in the causes, some in the signs and some share common symptoms with Amlapitta.
Clinical trial
Some Observations We have recently attempted to evaluate the role of certain indigenous measures in promotion of certain life style disorders.
Aims & Objectives
Clinical evaluation of the efficiacy of kamdudha rasa and drakshasava in amalpitta.
To provide safe, effective and cheap ayurvedic regimen for amalpitta by comparing the efficiacy of both the drugs.
Selection of Cases
40 Patients were randomly selected from My OPD of dac . Follow up was done weekly for a month.
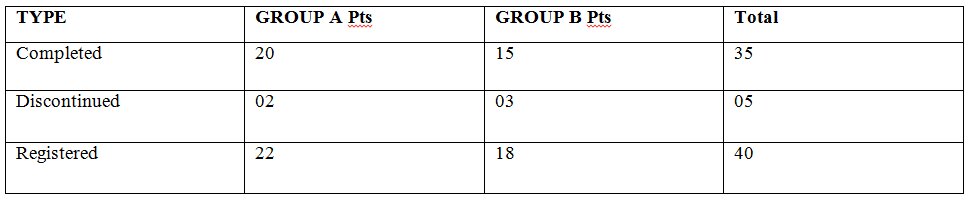
Registered patients: Table 6.
Table 6:
Inclusion criteria:
- Belonging to age group 18-60 years
- Chronicity less than 7 years
- Uncomplicated cases of amalpitta
Exclusion criteria:
- Uncontrolled diabetes mellitus
- Pregnancy
- Peptic ulcer
- Tuberculosis
- Malignany
- Chronic depression or related psychosomatic disorders
Criteria of Assessment
From the above table, it is clear that Amla rasa sevana taking persons were 22, Lavana rasa sevana persons were 20, Irregular diet takers were 15, Addiction of tea were present in 17 while on the other hand persons having Addiction of smoking and tobacco on individual level were 7 each, Day time sleepers were 18, Khandita nidra persons were 12, Krura kostha persons were 15. those on Abhishyandi bhojana were 15, persons taking Atiushan bhojana were 13, Vegavidharana persons were 13 and those with Krodha as dominant feature were 12.while on the other hand, if we look at the group b Amla rasa sevana taking persons were 16, Lavana rasa sevana persons were 17, Irregular diettakers were 8, Addiction of tea were present in 15 while on the other hand persons having Addiction of smoking were 9 and tobacco addiction persons were 8, Day time sleepers were 15, Khandita nidra persons were 10, Krura kostha persons were 9. Those persons who were on Abhishyandi bhojana were 10, persons taking Atiushan bhojana were 13, Vegavidharana persons were 10 and those with Krodha as dominant feature were 10.From the above table, it is clear that Amla rasa sevana taking persons were 22, Lavana rasa sevana persons were 20, Irregular diet takers were 15, Addiction of tea were present in 17 while on the other hand persons having Addiction of smoking and tobacco on individual level were 7 each, Day time sleepers were 18, Khandita nidra persons were 12, Krura kostha persons were 15. those on Abhishyandi bhojana were 15, persons taking Atiushan bhojana were 13, Vegavidharana persons were 13 and those with Krodha as dominant feature were 12.while on the other hand, if we look at the group b Amla rasa sevana taking persons were 16, Lavana rasa sevana persons were 17, Irregular diettakers were 8, Addiction of tea were present in 15 while on the other hand persons having Addiction of smoking were 9 and tobacco addiction persons were 8, Day time sleepers were 15, Khandita nidra persons were 10, Krura kostha persons were 9. Those persons who were on Abhishyandi bhojana were 10, persons taking Atiushan bhojana were 13, Vegavidharana persons were 10 and those with Krodha as dominant feature were 10.Results were assessed with regard to improvement in clinical findings. Changes observed in sign and symptoms were assessed by adopting suitable scoring methods and objectives symptoms by using appropriate clinical tools. All the selected common clinical presentation (Subjective criteria) of amalpitta are as:
- Amal tikta udgar (bitter and soul belching)
- Hrid kantha daha (burning sensation)
- Utklesha (nausea)
- Aruchi (loss of appetite)
- Shirashoola (Headache)
- Vibandha (constipation/hard stools)
- Gaurav (working capacity) altered
Besides these, it was compared with agnibala, rogabala and dehbala of the patient. Scoring thus given in each cardinal clinical finding mentioned above is as:-
- No sign
- Mild
- Moderate
- Severe
Objective criteria:-
- Hb, WBC & ESR
- Barium meal x ray for stomach/duodenum or endoscopy wheresoever necessary (not required in all cases)
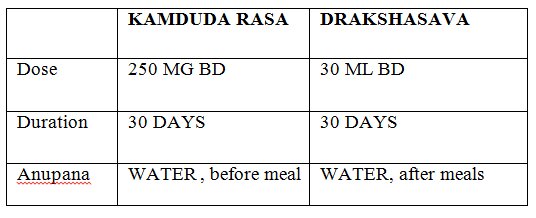
Drug details:- Table 7.
Table 7:
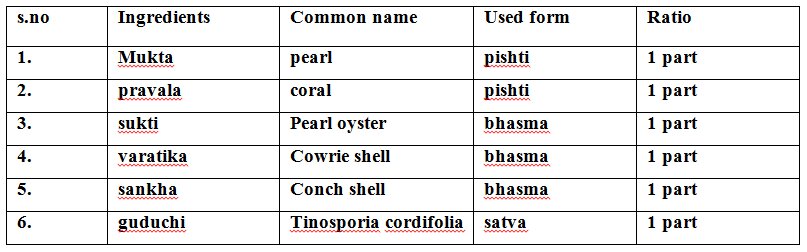
Ingredients of Kamdudha Rasa:- Table 8.
Table 8:
Overall assessment:-
Grade1-complete remission(100%)
Grade 2- marked improvement(75%-99.9%)
Grade 3-moderate(50% - 75%)
Grade 4- mild improvement(25%- 50%)
Grade 5 – unimproved(0%-25%)
Statistical Analysis:-
Paired “t” test for comparing means of cardinal symptoms of amalpitta was carried out at P<0.05, P<.01, P
Obtained results interpreted as:--
Insignificant P>0.05, significant P
1. Observation of Nidana sevana in patients of amalpitta:- Table 9.
Table 9:
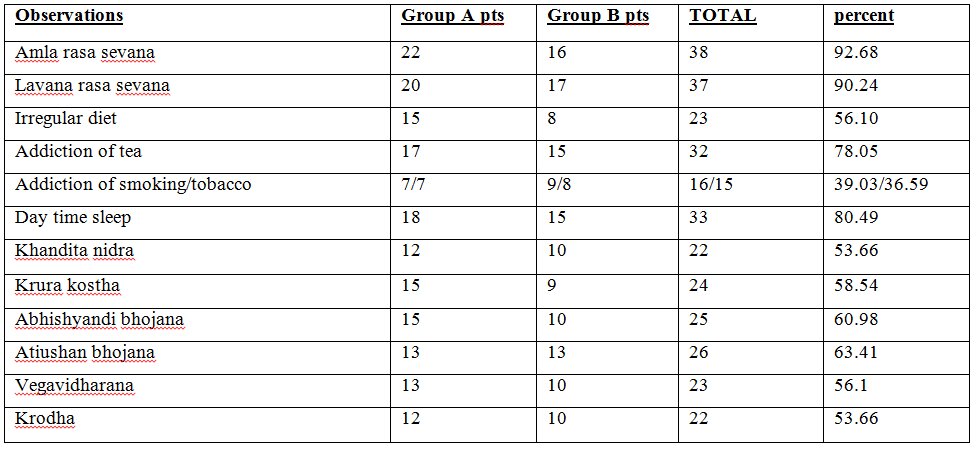
From the above table, it is clear that Amla rasa sevana taking persons were 22, Lavana rasa sevana persons were 20, Irregular diet takers were 15, Addiction of tea were present in 17 while on the other hand persons having Addiction of smoking and tobacco on individual level were 7 each, Day time sleepers were 18, Khandita nidra persons were 12, Krura kostha persons were 15. those on Abhishyandi bhojana were 15, persons taking Atiushan bhojana were 13, Vegavidharana persons were 13 and those with Krodha as dominant feature were 12.while on the other hand, if we look at the group b Amla rasa sevana taking persons were 16, Lavana rasa sevana persons were 17, Irregular diettakers were 8, Addiction of tea were present in 15 while on the other hand persons having Addiction of smoking were 9 and tobacco addiction persons were 8, Day time sleepers were 15, Khandita nidra persons were 10, Krura kostha persons were 9. Those persons who were on Abhishyandi bhojana were 10, persons taking Atiushan bhojana were 13, Vegavidharana persons were 10 and those with Krodha as dominant feature were 10.
2. Observation of cardinal symptoms in amalpitta patients:- Table 10.
Table 10:
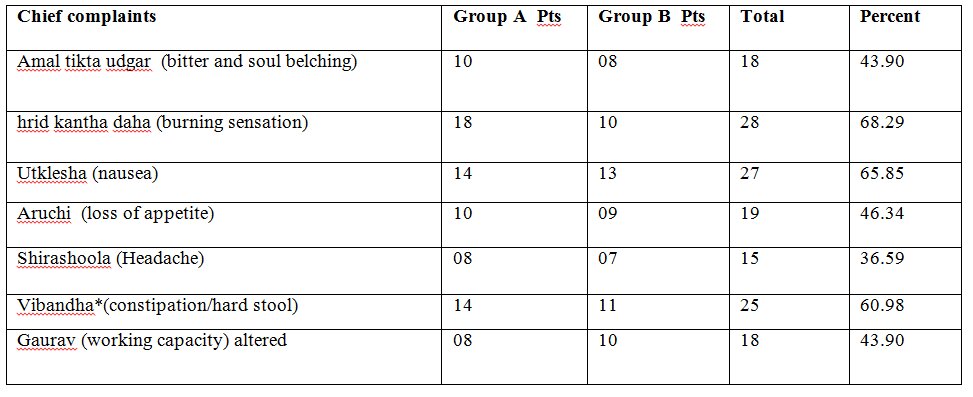
From the above table, it is cleared that in group A, Patients complaining of Amal tikta udgar (bitter and soul belching) were 10, hrid kantha daha (burning sensation) were 18 and the patients with Utklesha (nausea) as dominant feature were 14. similarily those with Aruchi (loss of appetite) were 10 , patients with Shirashoola (Headache) were 08 and the patients having Vibandha* (constipation/hard stool) as cardinal symptom were 14, while with that of Gaurav (working capacity) altered were 08 in number. In the similar way if we take look at group B, we will find that Patients complaining of Amal tikta udgar (bitter and soul belching) were 8, hrid kantha daha (burning sensation) were 10 and the patients with Utklesha (nausea) as dominant feature were 13. similarily those with Aruchi (loss of appetite) were 9, patients with Shirashoola (Headache) were 7 and the patients having Vibandha* (constipation/hard stool) as cardinal symptom were 11, while with that of Gaurav (working capacity) altered were 10 in number.
3. Effect of kamdudha rasa in amalpitta patients:- Table 11.
Table 11:
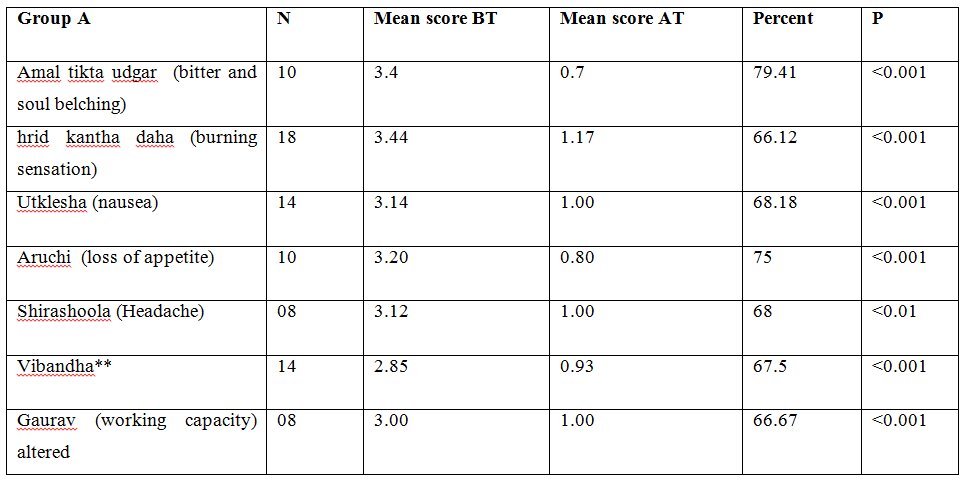
From the above table it is clear that in Group A, Amal tikta udgar (bitter and soul belching) which were 10 in number had their mean score reduced from 3.4 to 0.7. in the same way 18 patients with hrid kantha daha (burning sensation) whose mean score earlier was 3.44 got reduced to 1.17, 14 patients of Utklesha (nausea) had their mean score reduced from 3.14 to 1.00, 10 total patients of Aruchi (loss of appetite) got their mean score reduced from 3.20 to 0.80, 8 patients of Shirashoola (Headache) had their mean score reduced from 3.12 to 1.00, 14 patients of Vibandha had their mean score reduced from 2.85 to 0.93 and the last 8 patients with chief complaint of Gaurav (working capacity) altered had their mean score reduced from 3.00 to 1.00.
4. Effect of drakshasava in amalpitta patients: Table 12.
Table 12:
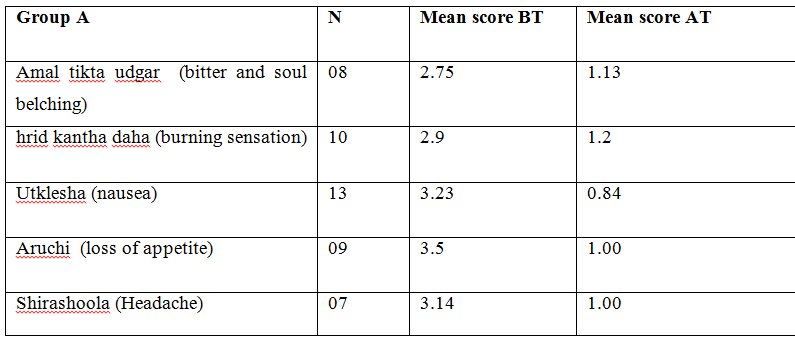
From the above table, it is clear that in Group B, Amal tikta udgar (bitter and soul belching) which were 8 in number had their mean score reduced from 2.75 to 1.13. in the same way 10 patients with hrid kantha daha (burning sensation) whose mean score earlier was 2.9 got reduced to 1.2, 13 patients of Utklesha (nausea) had their mean score reduced from 3.23 to 0.84, 9 total patients of Aruchi (loss of appetite) got their mean score reduced from 3.5 to 1.00 & 7 patients of Shirashoola (Headache)had their mean score reduced from 3.14 to 1.00.
5. Overall effect of Drakshasava on Rogabala, Agnibala and Dehabala:- Table 13.
Table 13:
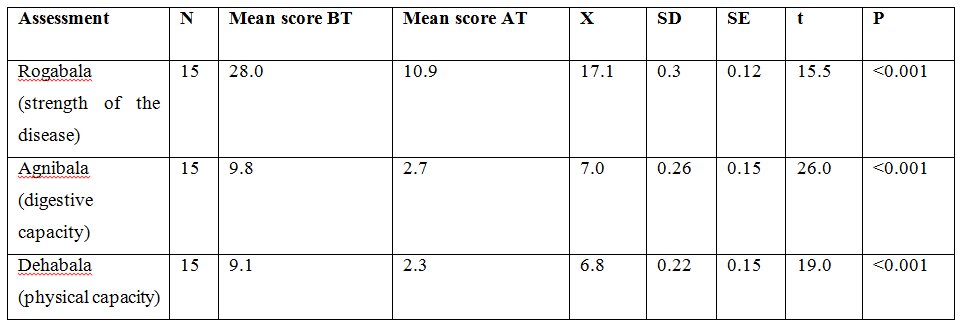
From the above table, it is clear that in 15 patients, rogabala(strength of the disease) had their mean score reduced from 28.0 to 10.9. In the same way in 15 patients, agnibala(digestive capacity) had their mean score reduced from 9.8 to 2.7 & 15 patients of dehabala (physical capacity) had their mean score reduced from 9.1 to 2.3 .
6. Overall effect of kamdudha rasa on Rogabala, Agnibala and Dehabala: Table 14.
Table 14:
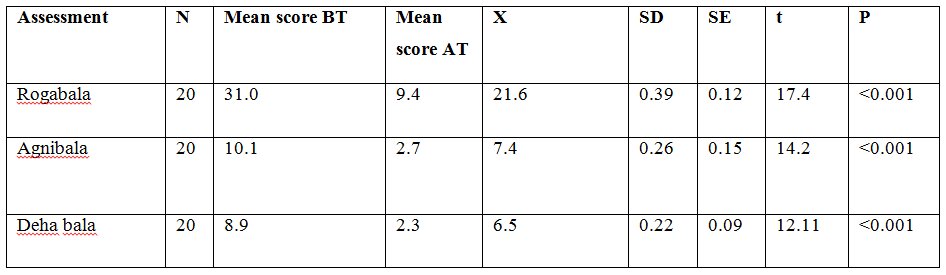
From the above table, overall effect of kamdudha rasa on Rogabala, Agnibala and Dehabala is observed as that in 20 patients, rogabala(strength of the disease) had their mean score reduced from 31 to 9.4 . In the same way in 20 patients, agnibala(digestive capacity) had their mean score reduced from 10.1 to 2.7 & 20 patients of dehabala (physical capacity) had their mean score reduced from 8.9 to 2.3 .
Overall effect of the medicine:- Table 15.
Table 15:
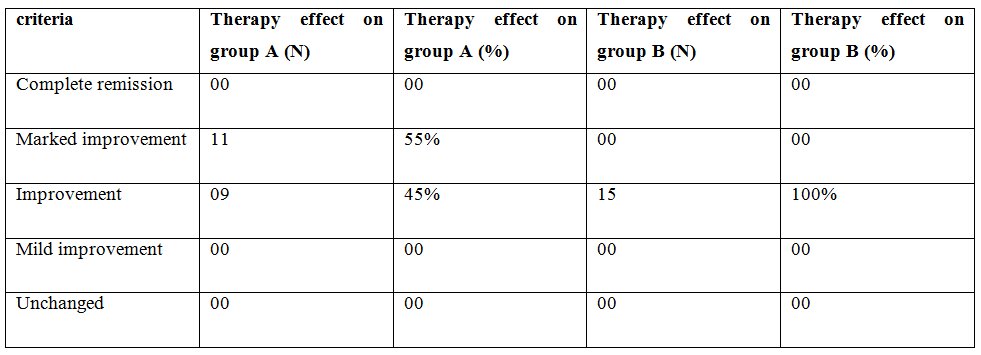
Effect of therapy:-
Kamduda rasa shows better result in symptoms such as kanthrid daha (burning sensation) and amlo tikta udgara (bitter and soul belching). Feeling of well being, quality of sleep and dehabala (physical capacity) also improved more in group A. While drakshasava shows better results in gaurava (being lazy), vibanda (constipation) and shirashoola (headache).
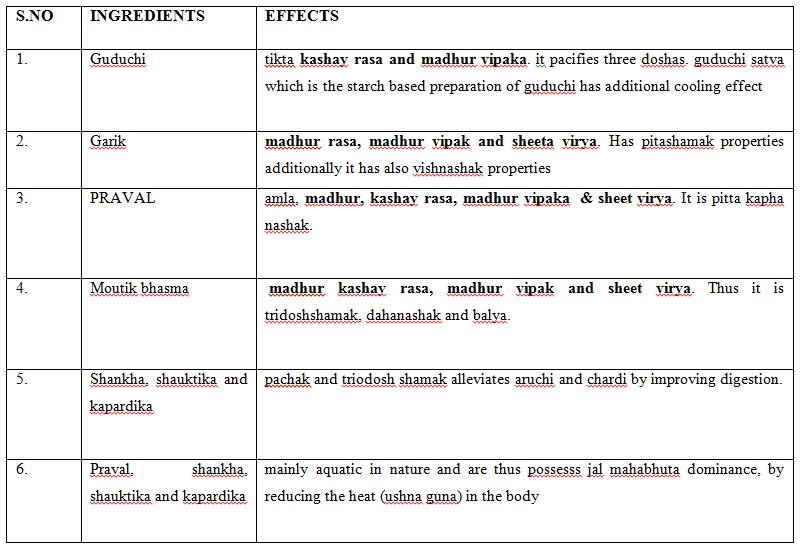
Probable mode of action of kamduda rasa:- Table 16.
Table 16:
Probable mode of action of drakshasava:-
In Drakshasava, main ingredient is raisin and that besides being mild laxative properties also stimulates bile from the liver, which is alkaline in nature and helps to neutralizes the excess stomach acid before it enters small intestine and in this way it is also helpful to improves digestion and increase the secretion of pitta in the stomach and bile salts from the liver, besides its elimination, which helps to reduce pitta agravation too. we can understand it very well that the drug used might not directly influence your body weight, instead it corrects appetite and digestion, which in turn might likely help to increase weight in underweight and malnourished people. If we understand it in modern view, we can find that Raisins present in this drug contains a high level of beta carbolines that might exhibit potential activity as MAO inhibitors, which act as a powerful antidepressant.
Discussion
- Basically simple agnimandya leads to vidagdhajirna in the initial stages, if neglected leads to amalpitta.
- Charaka has not mentioned disease amlapitta seperately even though he quoted word amlapitta several times.
- Charaka while describing nanatamaja vyadhis, included pittaj diseases such as dahaka, dhumaka, amlaka and vidaha. These are seen in APD and indicate pittolbana condition.
- Sushruta and vagbata have not mentioned the word amlapitta. Kashyapa was the first to describe it along with its treatment.
Conclusion
Conclusion is that prediction which can be done on the basis of results which are obtained from the present study.
Conclusions drawn after systemic open clinical trial on 40 pts are as follows:-
- Amlapitta showed its direct impact on annavaha srotasa.
- Agnimandya was present in majority of patients.
- Present lifestyle that has disturbed the food habits gives rise to agnimandya, vidagdhajirna annd finally leads to amlapitta.
- Socioeconomic condition, mental stress and strain play an important role in causing and aggravating the disease. As a result of the economic and social burdens of Urdhwaga Amlapitta, it is important for patients to have access to diet and lifestyle modifications
- Kamdudha rasa showed better result.
- Maximum number of patients were reported in 3rd-4th decade of life. most of them were females.
- The results of the survey study suggest that unwholesome diet, fast and stressful lifestyle with sedentary habits play an important role in the manifestation of this disease. Currently, research in this area is minimal.
- The results of the survey study suggest that unwholesome diet, fast and stressful lifestyle with sedentary habits play an important role in the manifestation of this disease. Currently, research in this area is minimal.
Scope of Further Study
- In future further scientific study is necessary.
- The study needs to be conducted seperately on h pylori positive and negative patients of the disease with different combinations, alterations in doses and the estimate duration of treatment, so that the amalpitta can be totally eliminated from the body.
